We know that a variety of life experiences can lead to opioid-exposed pregnancies. Some of the more common pathways include women with active addictions to opioids, and who may or may not be receiving opioids through medical means; women in recovery enrolled in a medication-assisted treatment program and who are taking methadone or buprenorphine as prescribed; and women who experience chronic pain and are taking opioids as prescribed.
Chronic Pain, Opioids and Pregnancy
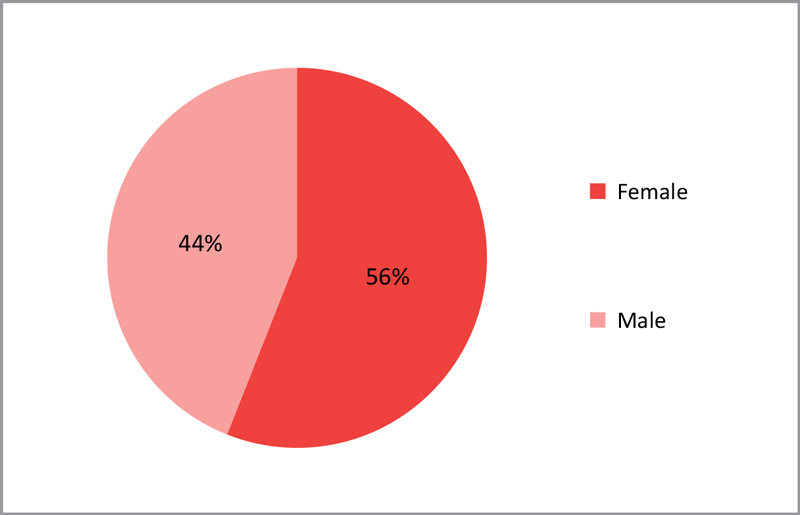
Studies have found that women are more likely to experience chronic pain than men. Conditions that women are commonly diagnosed with that cause chronic pain include fibromyalgia, irritable bowel syndrome, and migraine headaches. Women are more likely to be prescribed prescription opioids and to be given higher doses than men.
Chronic pain, by the way, isn’t just acute pain that doesn’t go away after a few months; it’s a transformation of the nervous system that can literally shrink the brain.[1],[2]
Women of child-bearing age who experience chronic pain may be prescribed opioids as a medical treatment to manage the pain and achieve a functional quality of life. They may, at some point, decide to have children. However, becoming pregnant and starting a family will not cure the cause of the chronic pain, and changing physical stress and hormone levels might exacerbate some conditions. Chronic pain is a physical stressor and — if left untreated and unmanaged — contributes to lower functioning, poor nutrition and depression, which are significant risks for poor birth outcomes. A woman with chronic pain who chooses to become pregnant will need to consult with her health providers to determine her best plan for pain management. At times, the best plan might be to continue opioid medication. Women who are prescribed opioids for a pain condition and who do not have a concurrent substance use disorder, are not candidates for opioid treatment programs (OTP’s) as the result of pregnancy alone.. Substance use treatment providers cannot accept patients for pain management alone, even if that management has led to a physical dependence.
Notably, people, including women who are pregnant, can experience physical dependence of opioids without having an opioid use disorder. Women may become physically dependent on prescription opioids more quickly than men.[6]
Physical dependence occurs because of normal adaptations to chronic exposure to a drug. Those who are physically drug dependent usually experience withdrawal symptoms when the drug is abruptly discontinued. They often develop a tolerance to the drug and require higher doses for the same effect.[6]
Women with chronic pain may or may not share some of the same struggles of the women who have an opioid use disorder such as a history of physical and/or sexual trauma, co-occurring mental health diagnosis, use of other substances such as alcohol or tobacco. Women who have experienced intimate interpersonal violence in their lifetimes are more likely to experience chronic pain.[3] The landmark Adverse Childhood Experiences (ACE) study revealed the correlation between childhood stress and trauma and later health difficulties including, for women, unintended pregnancies, sexually transmitted infections and fetal death.[4] Histories of trauma and violence should be taken into consideration when considering how best to support a woman and her pregnancy.[5]
Opioid Use Disorders
Many women in treatment for opioid use disorders describe a common pathway that began with opioids prescribed for an injury or chronic pain and ended with an opioid use disorder. In the beginning, the women took the medication as prescribed, but over time, most found they needed to increase the number of pills or frequency of their dose to achieve the same effect. Taking opioids over even over a short of time can create physical dependence, which can result in withdrawal if they are stopped. If not consulting with the prescriber, this can lead to ‘misuse’ Other factors often contribute to misuse of prescription opioids, including a woman’s history of trauma, co-occurring mental health issues, a history of addiction, or genetic vulnerability – all of which can affect the same woman. As with other substance use disorders, if left unaddressed and untreated, misuse of prescription drugs may progress to become a chronic disease. As the disease progresses, women may see multiple doctors for real or perceived pain complaints to obtain prescriptions for opioids. When prescribed medications cannot be obtained, they may turn to seeking illicit opioids. Cost of opioids dispensed through pharmacies typically ranges from $1–$3 a pill, whereas the street value of opioids can exceed $60 a pill. The high street cost of prescription medications may lead a woman to a cheaper alternative, which is often heroin.
Addiction involving opioids is classified as “opioid use disorder” based on the criteria of the 2013 Diagnostic and Statistical Manual of Mental Disorders (DSM-5)[6]. This disorder can range from mild to severe. The primary characteristics of a substance use disorder are described by the American Society of Addiction Medicine as
…a chronic disease of the brain reward, motivation, memory and related circuitry. It can be complicated by comorbid physical and psychological conditions and influenced by genetic and environmental elements.[7]
Similar to all substance use disorders, an opioid use disorder is a chronic disease that can affect any person, regardless of income level, race/ethnicity, education, or beliefs.
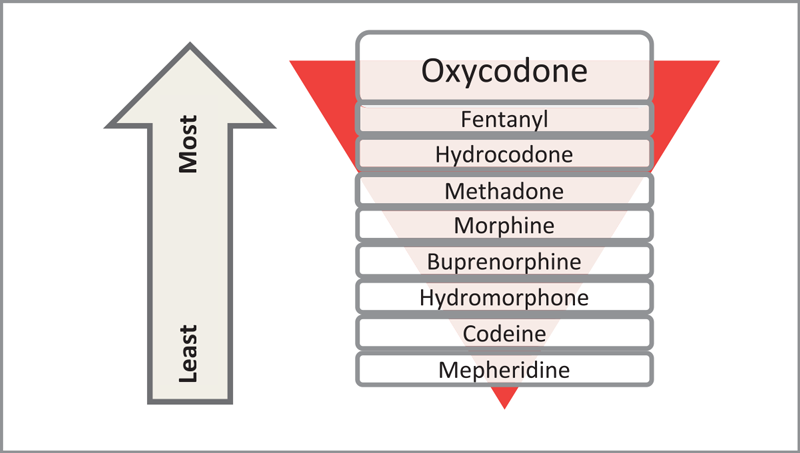
The prescription opioids include hydrocodone, fentanyl, oxycodone, and the controlled-release form of oxycodone (OxyContin®). The use of heroin, a semi-synthetic opioid with a rapid onset of effect, is increasing throughout North Carolina.[8] Although heroin is typically injected, an increasing number of people are inhaling or smoking heroin. Individuals with opioid use disorders often report using other substances as well, including, marijuana, alcohol and tobacco.
Whether naturally occurring or lab-created, all opioids work by directly affecting the central nervous system. Opioids stimulate the opiate receptors in the brain, producing effects that range from euphoria and pain relief to respiratory depression and nausea. Chronic use of opioids is associated with drug tolerance, meaning higher doses of the drug are required to obtain the same effect. Tolerance leads to physical dependence. The chronic use of opioids changes the neuro-chemical balance in the central nervous system, and the sudden absence of the drug triggers a withdrawal syndrome. Opioid withdrawal is characterized by a variety of symptoms including agitation, nasal congestion, yawning, muscle cramps, diarrhea, nausea, vomiting, and depression. The extreme physical discomfort of the withdrawal experience can prompt resumption of use.
The standard of care for individuals with an opioid use disorder is medication-assisted treatment (MAT) with opioid-agonists in conjunction with counseling and supportive services. Methadone and buprenorphine are the most commonly prescribed medications for opioid use disorders. Long-term research has demonstrated the efficacy of MAT for opioid use disorders. Evidence has shown that treatment including medication results in longer sustained recovery from addiction and improved quality of life. The efficacy of MAT also holds true for women who are pregnant.[9]
Opioid Use and Pregnancy
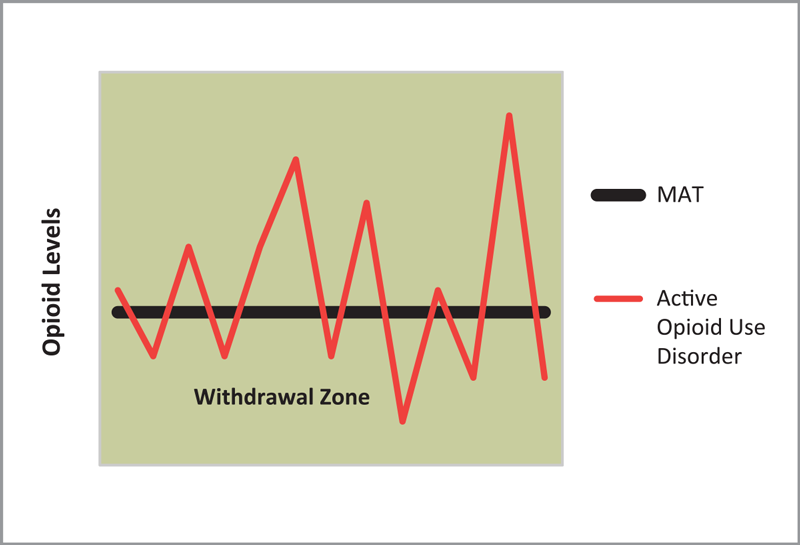
When a pregnant woman with opioid dependence, which can include an opioid use disorder, experiences a cycle of opioid use and withdrawal, the physical effects are particularly problematic to the developing fetus. Minimal disruption in the level of opioids during is ideal, so as not to cause withdrawal in the fetus. Repetitive patterns of use and withdrawal reduces the blood flow to the placenta, lowering the supply of oxygen available to the fetus and negatively affecting development. The consequences to the fetus include increased risk of prematurity, low birth weight, and fetal death. Thus, engaging pregnant women with opioid use disorders in comprehensive services, including prenatal care, is essential for positive birth outcomes.
Since the 1970s, the standard of care for pregnant women with an opioid use disorder has been medication-assisted treatment (MAT) with methadone. The efficacy of methadone as one element of comprehensive treatment services has been widely acknowledged and endorsed as a highly effective tool in recovery.[10],[11],[12] Comprehensive treatment services include case-management, life skills and childcare.[13] At appropriate dosages, methadone, a synthetic opioid, eliminates withdrawal symptoms, reduces cravings for the substance of choice, and blocks the euphoric effects of any other opioids ingested. Another benefit of methadone is the drug’s stability and its long half-life, that is, the amount of time it takes for half of the medication to be eliminated from the blood stream. The long half-life of methadone and the predictable dosing used in MAT prevents fluctuating opioid levels in the fetus, which contributes to a longer term pregnancy and improved fetal growth.
As a woman’s pregnancy progresses, her body will metabolize methadone more rapidly and higher doses are typically required to continue MAT effectiveness. Although some early reports suggested the dosage amount of methadone correlated with both the occurrence and the severity of neonatal withdrawal, this relationship has not been found in more recent evidence.[14] It is well understood that lowering the dose of methadone during pregnancy can trigger physical withdrawal symptoms and might lead to increased use of illicit drugs, exposing both mother and fetus to greater levels of health risk and harm.
Buprenorphine, a partial opioid-agonist, has been approved by the U.S. Food and Drug Administration (FDA) for the treatment of opioid addiction in an outpatient office setting. The FDA has established five categories indicating the potential of a drug to cause birth defects when used during pregnancy (Categories A, B, C, D, X). Buprenorphine is a Pregnancy Category C medication in pregnancy, meaning there is limited data, but the potential benefits may warrant use of the drug. Physicians are encouraged to do a risk-benefit analysis in considering the use of buprenorphine in the treatment of an opioid use disorder with a woman who is pregnant.[15] Preliminary research of buprenorphine use during pregnancy is promising.[16]
In addition to the health concerns related to opioid withdrawal, women with opioid use disorders are also at elevated risk for hepatitis B, hepatitis C, and HIV transmission through needle sharing and unsafe sexual practices. Screening for these infections should be done by the woman’s medical provider, and in the case of HIV infection, treatment should be initiated.
Over the years we have learned from the women entering treatment for substance use disorders in North Carolina, that their needs are complex. The analysis of 10 years of data from the North Carolina Perinatal and Maternal Substance Abuse Initiative has produced the following picture of this population:
- 60% of women in treatment report a history of intimate partner violence;
- 53% have experienced sexual abuse;
- 70% of women have a family history of substance abuse;
- 36% are involved with the child welfare system, with most seeking to regain custody of one or more children; and
- 70% need assistance with transportation for medical appointments for mother and/or children, social services appointments, behavioral health services, housing assistance, or vocational aspects of their treatment plan.[17]
As this statistical picture illustrates, women and their families are involved in multiple systems, which further compounds their challenges given the lack of uniform, comprehensive services. The challenges of dealing with multiple systems can be overwhelming.
Services may be fragmented, requiring a woman to negotiate a maze of service agencies to obtain assistance for housing, transportation, child care, substance abuse treatment, vocational training, education, and medical care. In addition, many agencies have requirements that conflict with each other or endorse repetitive intake processes, including different forms that gather the same information. Overall, these simultaneous demands can discourage a woman, particularly when seeking treatment or during early recovery.[11]
This guidance document seeks to promote collaborative approaches that support women’s access to treatment and recovery from opioid use disorder, and in ways that enable the focus to be on the health and well-being of infant and mother.
Opioid Overdose Risk
Any woman taking opioids is at risk of fatal overdose. The rate of fatal overdoses among women has risen dramatically.[18] Opioids depress the central nervous system, and when mixed with other substances including alcohol or other prescribed medication such as anti-anxiety medication (e.g., benzodiazepines) result in an increased risk of overdose. Women should be made aware of their risks for overdose, how to prevent an overdose, and safety steps to be prepared in case of an overdose.
The initial effects of an opioid overdose can be reversed with the prescription medication naloxone. Having prescribed naloxone on hand — and making sure a friend or family member knows the location, can quickly access the medication, and knows the dose to administer — can be an important piece of preventing a fatal overdose. Being prepared by having access to naloxone is considered one part of a continuum of substance use disorder and health services.[19] Naloxone has no psychoactive effects and does not have any potential for abuse.[20]
Naloxone can safely be used to manage opioid overdose in pregnant women. The lowest dose to maintain spontaneous respiratory drive should be used to avoid triggering acute opioid withdrawal, which may cause fetal distress.[17]
Access to prescribed naloxone has expanded in North Carolina. In 2013, North Carolina enacted the Good Samaritan/Naloxone Access Law, protecting individuals involved in seeking medical care for a potential overdose victim from prosecution of drug related offenses. This legislation also limits civil liabilities of prescribers of naloxone, while acting in good faith, providing the prescription to persons at risk of experiencing an opioid overdose, a friend, family member or other person in a position to help.[21]
Community Care of North Carolina’s Project Lazarus, The North Carolina Harm Reduction Coalition, and other partners have worked to make naloxone available through as many avenues as possible including, but not limited to, community pharmacies, health departments, law enforcement officials, opioid treatment programs, and directly to patients via standing order.
For more information on preventing opioid overdoses see the SAMHSA Overdoses Kit and The North Carolina Harm Reduction Coalition.